Neuroendocrine System Overview
The neuroendocrine system includes the nervous and endocrine systems, which work together to regulate body functions.
According to the World Health Organization (WHO), Neuroendocrine Neoplasms (NENs) are classified as NETs (Neuroendocrine Tumors, which are less aggressive and also called carcinoids) and NECs (Neuroendocrine Carcinomas, which are more aggressive, including Small Cell Neuroendocrine Carcinoma and Large Cell Neuroendocrine Carcinoma).
Prevalence:
The most common site of Neuroendocrine Neoplasia (NEN) is the gastroenteropancreatic (GEP) region, which makes up about 55% to 70% of all cases.
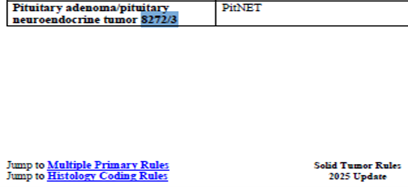
Coding Guidelines:
Starting in 2025 and forward, pituitary adenomas (PitNETs) must be coded as malignant.
Merkel cell carcinoma is a highly aggressive neuroendocrine skin cancer, sometimes found in major salivary glands. It can quickly metastasize early to lymph nodes, lungs, bones, and the brain.
Always specify the subtype for NECs; avoid coding as generic neuroendocrine, NOS if a specific subtype is available.
The most common types of neuroendocrine carcinomas are SCNEC and LCNEC, which stand for small cell neuroendocrine carcinoma and large cell neuroendocrine carcinoma, respectively. However, sometimes you may need to code for Combined Large Cell Neuroendocrine or Combined Small Cell Neuroendocrine, or other more specific subtypes.
Functional vs. Non-Functional Tumors:
NENs can be either functional (hormone-secreting) or non-functional. Head and neck neuroendocrine tumors are typically non-functional and may include extra-adrenal pheochromocytomas (paragangliomas). These tumors can be found in the middle ear, the glomus jugulare, the carotid body, the vagal nerve, and the larynx.
Behavior Coding Changes:
Before January 1, 2021: Only malignant behavior was reported for certain paragangliomas.
After Jan 1, 2021: The term “malignant” is no longer mandatory, but behavior remains coded as malignant unless specified otherwise.
For 2026: A new related term was introduced: 8240/3 Middle ear neuroendocrine tumor.
Pheochromocytomas can also occur in children and may lead to hypertension, especially if they have a genetic syndrome that increases their risk of developing it.
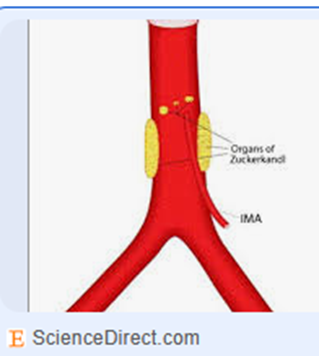
A paraganglioma or pheochromocytoma in the organ of Zuckerkandl (paraganglioma of the para-aortic body) is situated at the aortic bifurcation, where the aorta divides into the left and right common iliac arteries at the level of L4.
Other paragangliomas and pheochromocytomas can develop in the mediastinum, retroperitoneum, urinary bladder, and coccygeal body.
Treatment Coding:
Somatostatin analogs can be used in NETs (carcinoids), but are not effective in NECs.
Octreotide (Sandostatin) may be coded when used to shrink tumors or prevent their growth.
If you have a somatotroph (growth hormone) pituitary adenoma causing acromegaly, Octreotide can shrink the tumor.
Lanreotide (Somatuline) can be coded to treat the tumor, but should not be coded solely for managing symptoms of carcinoid syndrome.
Typically, Lanreotide is used to treat tumors in cases of acromegaly and thyrotrophic adenomas, as well as gastrointestinal and pancreatic neuroendocrine tumors (GEP NETs) that have metastasized and cannot be removed through surgery. It helps slow tumor growth.
Pasireotide is another somatostatin analog, and it should be coded.
Accurate classification and coding of neuroendocrine neoplasms are vital for effective cancer data management. Staying current with evolving guidelines ensures accurate data reporting.
Click on the tags below to see related articles: