Krukenberg Tumors
An in-depth review of Krukenberg Tumors
Introduction
Suppose you encounter a case of Ovarian Cancer. Upon further reading you see that there is also cancer of the stomach in this patient.
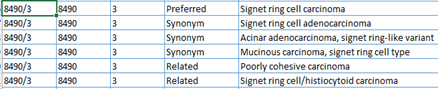
While our initial instinct might be to create two abstracts one for the ovarian cancer and another for the stomach cancer, it is important to consider the specific histology of the two cancer sites. Are they the same? If the histology indicates Signet-Ring Cell Adenocarcinoma, there may be more to the story requiring additional investigation.
A Krukenberg tumor is a Signet-Ring Cell Adenocarcinoma that has metastasized to the ovaries from a primary site, most commonly being the stomach or GI tract. Statistics indicate that the chances that the primary is in the stomach are extremely high, as most (50-59%) signet ring cell carcinomas are in the stomach in the pylorus area of the stomach.
The tumor's distinct "signet ring" cells, named for their unique appearance under a microscope, result from mucin accumulation pushing the nucleus to the cell's periphery giving the ring shape appearance.
If we find two sites with Signet Ring cell Adenocarcinoma histology, it is important to investigate the case more (especially if one of the sites is one or both ovaries). This rare histology is more common in younger patients and has a worse prognosis. Signs and Symptoms may be vague like other ovarian cancer primaries. They may include abdominal pain, bloating, weight loss, abdominal mass, intestinal obstruction.
Diagnostic Tests
A pelvic ultrasound or a CT scan may reveal a mass in the ovary or ovaries.
A biopsy to confirm the specific histology Signet Ring cell adenocarcinoma.
An endoscopy may be performed in the GI tract to look for a primary site.
Registrars should report on the primary site, not the metastatic site.
Age 27-65 years Usually < 50 years
More incidence in males than females
Asiatic countries have a higher incidence of this histology (up to 21%) as they have a higher incidence of stomach cancer.
Up to 80% of Krukenberg tumors are bilateral (both ovaries).
Possible Primary Sites
GI tract signet ring cell Adenocarcinomas: Stomach (56.8%), Colon (15.3%), Esophagus (4.7%), Rectum (4.3%), Small bowel (1.1%). Over 82% are in the Gastrointestinal tract! Even almost 90% in some literature.
Lung (3.1%), Pancreas (2.1%), Appendix (2% - 3%), Gallbladder/Biliary (1.6%), Breast (1.5% - 4%,) Urinary Bladder (1.3%), Ovary (<1%)
Treatments
Surgery
Chemotherapy, which may include HIPEC (Hyperthermic Intraperitoneal Chemotherapy). Palliative medical treatment to alleviate symptoms.
Since Krukenberg tumors are less responsive to chemotherapy, having surgery before chemotherapy increased responsiveness to chemotherapy. Furthermore, according to the National Institute of Health (NIH), Surgical removal of the metastatic tumor (metastasectomy) increases survival.
Prognosis
Krukenberg tumors diagnosed at the same time as the primary tumor (synchronous) have a shorter survival period than those diagnosed later than the primary site, signet ring adenocarcinoma (metachronous).
5-year relative survival rates:
Gastric cancer in general: 36.4%
Synchronous Krukenberg 9% in comparison to Metachronous Krukenberg 20%
Conclusion
When you encounter Signet-Ring Cell Adenocarcinoma in one or two ovaries, consider that the probabilities of this being a primary site are less than 1, while the probabilities of this being a Krukenberg metastatic site are very high, especially if you have another site with the same histology. Being the stomach the most common location, follow for another GI tract site.
Fritz, April International Classification of Diseases for Oncology. Third Edition. WHO
ICD-O-3.2 SEER ICD-O-3 Coding Materials
Copy-of-ICD-O-3.2_MFin_17042019_web.xls
Muhammad Aziz; Robert B. Killeen; Karen Carlson; Anup Kasi. Krukenbert Tumor. StatPearls Publishing; 2025 January. National Library of Medicine.
Click on the tags below to see related articles: